THEHOPE
Traditional HEalers working with primary care and mental Health for early interventiOn in psychosis in young PErson: intervention development and feasibility study
This project is led by Professor Saeed Farooq
The Global Mental Health research team at KEELE University School of Medicine have been awarded funding by the Medical Research Council to carry out a 30-month research project in Pakistan which aims to develop a culturally appropriate and targeted intervention for a young person first experiencing psychotic symptoms. The project is in joint sponsorship with Khyber Medical University (KMU), Pakistan.
In low- and middle-income countries (LMICs), more than half of patients with First Episode Psychosis (FEP) initially seek treatment from traditional and spiritual healers (TSH) as their first care. This contributes to an excessively long duration of untreated psychosis. It can take over two years for someone living in a LMIC to be diagnosed and treated for psychotic episodes – double the time it takes for someone in the UK. That's why Interventions involve TSHs to work collaboratively with primary care practitioners and psychiatrists.
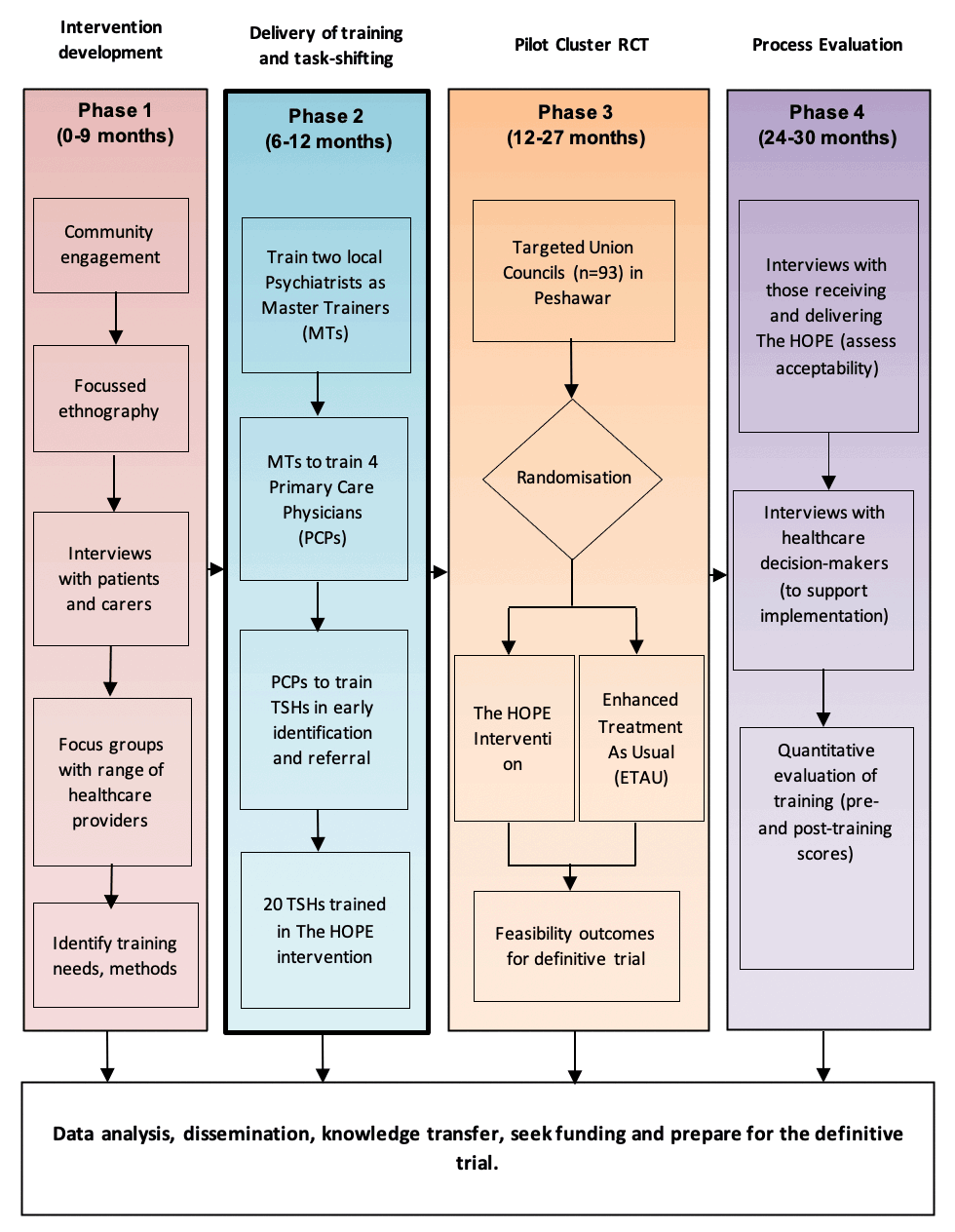
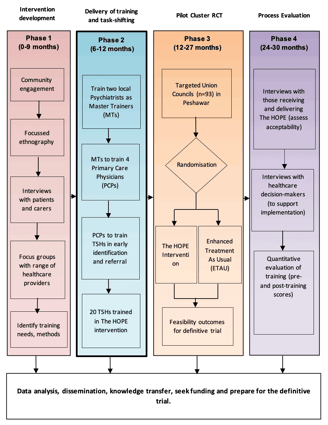
The study has developed and tested a model of working with traditional healers using a rigorous randomized controlled cluster feasibility trial with a nested qualitative study to assess study recruitment and acceptability of the intervention.
THEHOPE consist of four work packages:
Background and Study aims:
One in ten people experience a psychotic episode (delusion, hallucination) before 18 years of age. These experiences can be upsetting and, without adequate treatment, can have serious long-term effects (e.g. reduce quality of life, disrupt education, reduce long-term employment). Early treatment after a psychotic episode is vital to reduce long-term effects.
People living in Low-and Middle-Income Countries (LMICs) (e.g. Pakistan) experience poorer access to care compared to those in Higher Income Countries (e.g. UK, USA). It can take over 2 years for someone living in an LMIC to be diagnosed and treated for psychotic episodes. This is double the time it takes for someone in the UK.
Previous research about psychotic episodes in the Peshawar district of Pakistan found that people with mental health issues often sought help from traditional and spiritual healers (TSHs). These issues are commonly linked to superstition and/or spirits. Seeking help from TSHs is a key cause of delay in treatment for psychotic episodes.
Collaboration between TSHs and primary care has been shown to improve healthcare provision for health conditions, such as HIV/AIDS, but the same has not been evaluated for psychotic episodes, up to now.
The proposed program of research, called THEHOPE (traditional healers working with primary care and mental health for early intervention in psychosis), seeks to develop a new way of detecting and treating psychotic episodes among adolescents in Peshawar, Pakistan. This research strengthens collaboration between TSHs and primary care to improve healthcare for patients reporting these issues. By working with TSHs the researchers developed a new approach that is culturally sensitive and acceptable to local populations.
Study Hypothesis
This study evaluates the feasibility and acceptability of THEHOPE intervention by investigating the acceptability of task sharing, training procedures, and establishing pathways for referral and management of FEP. Specifically, the study aims to answer the following research questions;
1. Does involving traditional healers and primary care in early detection and treatment of First Episode Psychosis (FEP) lead to earlier detection and better management of First Episode Psychosis (FEP) compared to treatment as usual in a low and middle-income country (LMIC) setting?
2. Is it feasible and acceptable to establish care pathways for early detection and management of first episode psychosis in young person (FEP) for evidence-based management of FEP?
Ethics Approval(s)
1. Approved 16/08/2021, Keele University Faculty of Medicine and Health Sciences Research Ethics Committee (Keele University, Staffordshire, ST5 5BG, UK; +44 (0)1782 732000; health.ethics@keele.ac.uk), ref: MH210177
2. Approved 15/11/2022, National Bio Ethics Committee Pakistan (Health Research Institute, Shahrah-e-Jamhuriat, Off Constitution Avenue, Sector G-5/2, Islamabad, Pakistan; +92 (0)51 9224325; nbcpakistan@nih.org.pk), ref: 4-87/NBC-840/22/621
Study Design:
Pragmatic feasibility cluster pilot randomized controlled trial








